Sales Team
Project quotes, partnerships, implementation
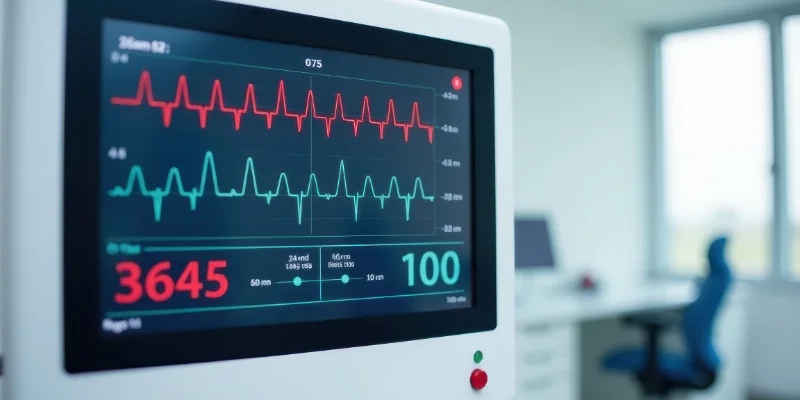
Have you ever wondered how many critical heart rate fluctuations go unnoticed between your doctor’s visits? This is where remote patient monitoring (RPM) is revolutionizing cardiac care by offering real-time visibility, continuous analysis, and immediate alerts that traditional monitoring simply cannot provide.
Heart rate is one of the most important indicators of cardiovascular health. Monitoring it continuously, accurately, and in real time enables early detection of abnormalities, better management of chronic conditions, and improved decision-making for clinicians. Remote patient monitoring (RPM) has emerged as a breakthrough in this space, providing continuous heart rate visibility without requiring patients to visit clinics frequently. With the rise of remote health monitoring, advanced wearables, and digital tools, heart rate tracking is now more accessible, precise, and proactive than ever.
Heart rate patterns reveal essential information about how well the heart is functioning. Whether at rest, during sleep, or under physical or emotional stress, changes in heart rate often indicate underlying conditions such as arrhythmias, atrial fibrillation, heart failure, or hypertension. Traditional monitoring, however, provides only periodic snapshots.
Continuous monitoring through technologies like a heart rate tracker, a heart rate tracker watch, or a wrist heart rate tracker allows clinicians to identify abnormalities that may be missed during short clinical visits. When this continuous tracking is integrated into remote health monitoring ecosystems, it supports preventive care, chronic disease management, and emergency detection more efficiently.
Remote patient monitoring is a technology-enabled system where patient data such as heart rate is collected through digital devices and transmitted securely to healthcare providers. By combining medical-grade sensors, mobile applications, and cloud platforms, RPM makes it possible to monitor a patient’s heart continuously.
Modern remote patient monitoring solutions integrate easily with a range of cardiac devices, helping providers gain access to real-time metrics. The combination of rpm software, smart sensors, and patient-friendly wearables ensures continuous data transmission, instant alerts, and preventive care interventions.
RPM transforms the traditional approach to cardiac care by providing measurements that reflect real-life scenarios rather than short-term readings obtained in a clinical setting. This helps clinicians diagnose more accurately and treat cardiac issues based on long-term data patterns.
Remote patient monitoring systems operate through a coordinated workflow that connects the patient, their monitoring devices, and the healthcare provider in real time. These systems leverage advanced sensors, connectivity technologies, analytics, and patient-facing digital tools to ensure continuous oversight of heart rate data. Below is a detailed breakdown of how the process works:
The foundation of the RPM process begins with accurate data collection. Patients use devices such as an activity tracker with heart rate, a heart rate tracker watch, or a wrist heart rate tracker equipped with optical sensors. These sensors use PPG (photoplethysmography) technology, where gentle LED light penetrates the skin and measures fluctuations in blood volume.
These fluctuations are then converted into numerical heart rate values, allowing the system to track resting heart rate, heart rate variability, and activity-related changes. Modern activity trackers that track heart rate can also capture additional vitals such as oxygen saturation, calorie burn, and sleep patterns, providing clinicians with a more complete picture of the patient's cardiovascular health.
Once collected, the data is transmitted securely to the care team’s monitoring platform. Most devices support multiple communication protocols, including:
This multi-channel approach ensures uninterrupted data flow. Every transmission is fully encrypted to protect patient privacy and comply with healthcare standards such as HIPAA. By maintaining constant connectivity, RPM systems eliminate data gaps and provide clinicians with reliable, real-time insights into the patient’s cardiovascular trends.
Once heart rate data reaches the platform, the remote patient monitoring software begins processing it using machine learning algorithms and predictive models. These intelligent tools evaluate:
If the system detects abnormalities such as tachycardia, arrhythmia, or unusually low heart rate, automated alerts are generated for the provider. Advanced RPM software can even triage alerts based on severity, ensuring that critical cases receive immediate attention. This level of proactive monitoring helps clinicians intervene early, reducing hospitalizations and preventing major cardiac complications.
Healthcare providers access a secure online dashboard where all data is aggregated and visualized. The dashboard presents:
These insights enable clinicians to make more informed decisions. For example, if an activity tracker with heart rate shows an increase in resting heart rate over several days, the provider can evaluate potential causes such as stress, medication side effects, or the onset of illness. The dashboard also integrates with EHRs, ensuring that patient records remain up-to-date without manual entry.
A key advantage of RPM is its ability to increase patient awareness. Through a heart rate tracker app, patients can view their daily heart rate patterns, receive reminders, track workouts, and get notified when readings fall outside safe limits.
This not only enhances their engagement but also encourages healthier behaviors such as regular exercise, hydration, and medication adherence. Many patients find that using a heart rate tracker or wearable helps them visualize progress, stay motivated, and communicate concerns more effectively with their care team.
Remote heart rate monitoring relies on a sophisticated blend of biomedical sensors, intelligent algorithms, mobile platforms, and secure cloud infrastructures. These technologies work together to convert raw physiological signals into actionable clinical insights. Modern RPM solutions use the same level of precision found in hospital-grade remote patient monitoring devices, making remote care both reliable and scalable. Below is a detailed explanation of the core technologies that enable advanced heart rate tracking:
PPG sensors are among the most widely used technologies in consumer and medical wearables. They are found in devices such as an activity tracker that tracks heart rate, a heart rate tracker watch, and various wrist heart rate tracker devices.
These sensors work by shining LED light into the skin and measuring changes in blood volume with each heartbeat. As the heart pumps blood, the amount of reflected light changes, helping the device calculate:
PPG technology has grown increasingly accurate thanks to improved optical design, multi-wavelength LEDs, better algorithms, and motion compensation features. As a result, even consumer-grade devices offer near-clinical accuracy during normal daily activities, contributing significantly to the reliability of remote patient monitoring systems.
While PPG sensors are ideal for continuous everyday monitoring, ECG/EKG sensors provide clinical-level diagnostics. These sensors are frequently used in:
Unlike PPG, ECG sensors directly measure the electrical activity of the heart, providing unmatched precision for detecting:
They are essential in remote health monitoring for high-risk cardiac patients because they capture detailed rhythm patterns that optical sensors cannot detect. ECG-based devices also integrate seamlessly with remote patient monitoring solutions, allowing clinicians to access long-term electrophysiological data without requiring in-person visits.
Artificial intelligence is the backbone of modern heart monitoring systems. AI tools analyze large volumes of heart rate data captured by devices from an activity tracker with heart rate to more advanced ECG monitors—and turn this data into meaningful insights.
AI enhances RPM systems by:
Furthermore, AI models continuously learn from patient-specific data, enabling personalized monitoring. This predictive capability makes RPM systems far more proactive than traditional episodic check-ups.
Mobile and cloud ecosystems power the communication layer of remote monitoring systems. Patients use a heart rate tracker app installed on their smartphones or tablets to track metrics, receive notifications, and communicate with their care team.
Simultaneously, cloud-based platforms manage:
Cloud technology ensures that large volumes of heart rate data captured by wearables can be uploaded, analyzed, and viewed instantly. It also supports integration with telehealth platforms, EHR systems, and other digital health solutions. This enables collaborative, patient-centered care where clinicians can make quicker decisions based on up-to-date information.
Together, these technologies make remote monitoring extremely reliable and effective. By combining advanced sensors, intelligent analytics, secure cloud infrastructure, and user-friendly mobile applications, RPM systems offer:
This integration ensures that both healthy individuals and chronic care patients benefit from consistent, precise, and proactive heart health monitoring—even from the comfort of their homes.

Modern remote heart rate monitoring depends on a wide range of advanced, patient-friendly devices. These tools not only capture accurate physiological data but also ensure seamless integration with digital RPM platforms. Below is a detailed look at the devices most commonly used in remote patient monitoring programs.
Smartwatches and fitness wearables are among the most widely used devices for remote heart rate monitoring. These act as both an activity tracker with heart rate and a daily wellness companion. Their convenience, affordability, and continuous monitoring capabilities make them ideal for both general users and patients with underlying conditions.
These devices can track:
Thanks to improved optical sensors, motion correction algorithms, and longer battery life, today’s wearables provide clinical-quality insights suitable for RPM environments.
For patients requiring high clinical precision—such as those with chronic cardiac arrhythmias, post-surgical recovery needs, or high cardiac risk medical-grade ECG patches play a crucial role.
These devices:
Because ECG patches measure electrical activity rather than optical changes, they are highly accurate for detecting arrhythmias such as AFib, premature beats, bradycardia, and tachycardia. Their seamless integration with RPM systems allows clinicians to receive instant alerts about critical heart rhythm abnormalities.
Chest straps are considered one of the most reliable non-invasive tools for ECG-level accuracy. These devices are widely used in cardiac rehabilitation programs, fitness training, and remote monitoring setups that require highly precise data.
Key benefits include:
Because chest straps sit close to the heart and remain stable during movement, they excel in both clinical and athletic contexts.
Biosensors offer a comprehensive approach to remote patient monitoring by measuring multiple vital signs simultaneously. They are especially valuable for complex or high-risk patients.
These devices capture:
Multi-vital biosensors support early detection of severe conditions such as respiratory distress, circulatory issues, cardiac decompensation, and post-operative complications. Their ability to combine multiple physiological signals strengthens the reliability of RPM insights.
A heart rate tracker app acts as the communication bridge between the patient and the clinician. These apps are designed to sync seamlessly with various wearable devices such as smartwatches, biosensors, chest straps, and fitness trackers.
Features typically include:
These apps empower patients by giving them continuous access to their heart health data, improving engagement and overall adherence to treatment plans.
Traditional heart monitoring—conducted only during medical visits—often leaves large gaps. Symptoms such as nighttime arrhythmias, stress-induced spikes, or sudden drops in heart rate may go undetected. Remote heart monitoring removes these gaps and provides a full, real-time picture of heart performance.
With continuous monitoring and devices like a heart rate tracker watch, clinicians can catch fluctuations the moment they happen, making RPM far more effective than episodic clinic-based readings.
Accuracy is significantly improved due to several factors:
![]()
Unlike in-clinic checkups, RPM devices collect thousands of data points per day. This:
Continuous data makes diagnoses far more accurate and reliable.
RPM systems enhance accuracy through advanced analytics. AI assesses:
This reduces false positives and identifies critical issues early.
Heart rate readings are enriched when systems also track:
When activity patterns correlate with pulse fluctuations, clinicians can better understand the root cause of irregularities.
Many RPM systems combine both optical (PPG) and electrical (ECG) data. This hybrid approach delivers:
This multi-tech synergy increases overall reliability.
All RPM data is stored securely using advanced patient monitoring software. Long-term storage allows providers to:
This historical perspective is invaluable for managing chronic heart conditions.
Clinical Benefits of RPM-Based Heart Rate Tracking
Remote patient monitoring (RPM) has transformed how clinicians observe cardiovascular function by enabling continuous, real-time heart rate assessment outside traditional clinical environments. This advancement enhances diagnostic accuracy, supports better medical decision-making, and improves long-term patient outcomes. Below are the primary clinical benefits of heart-rate-focused RPM systems.
One of the biggest advantages of RPM is its ability to catch early warning signs that are often missed during occasional clinic visits. By continuously collecting data through a heart rate tracker, chest strap, smartwatch, or wrist heart rate tracker, RPM enables clinicians to recognize emerging abnormalities long before they escalate.
RPM systems help detect:
These detections are supported by RPM dashboards that send instant alerts, enabling rapid clinical intervention and reducing the risk of cardiac emergencies.
Patients with chronic cardiovascular conditions often require long-term monitoring to prevent deterioration. RPM provides clinicians with continuous streams of heart rate data, helping them monitor conditions such as:
This consistent monitoring makes it easier to adjust treatment regimens, track medication adherence, monitor fluid retention, and detect early symptoms of cardiac decompensation. By linking activity levels, sleep patterns, and heart rate trends, RPM provides a holistic view of a patient’s cardiovascular health.
One of the measurable benefits of remote health monitoring is its impact on hospital utilization. By detecting early warning signs and offering continuous oversight, RPM significantly decreases:
This is made possible through swift clinician notifications delivered via remote patient monitoring solutions, enabling intervention before the situation worsens.
Personalization is at the heart of modern cardiac care. RPM supplies long-term, high-volume heart rate data that gives clinicians deep insight into how a patient’s heart behaves under different circumstances—resting, sleeping, exercising, or experiencing emotional stress.
With this level of detail, clinicians can design individualized treatment strategies based on:
Longitudinal data also enables early trend recognition, allowing physicians to adapt treatment plans proactively rather than reactively.

Heart rate metrics become even more meaningful when correlated with other vitals. Modern RPM systems combine heart rate sensors with technologies that track:
This synergy creates a comprehensive clinical picture.
These integrated insights form the foundation of advanced remote patient monitoring integration strategies used in modern healthcare environments.
Many organizations enhance these capabilities through remote patient monitoring software development that aligns with their clinical workflows and interoperability requirements.
Heart rate tracking through RPM supports a wide range of clinical and lifestyle applications. Below are key use cases where RPM adds significant value.
Patients recovering from a heart attack, cardiac surgery, or stent placement require safe, guided exercise programs. RPM helps clinicians:
This enables safer rehabilitation without requiring daily in-person visits.
Managing long-term cardiac disease requires constant vigilance. RPM supports:
Patients with hypertension or heart failure benefit particularly from this continuous oversight.
Elderly patients often struggle with mobility and frequent clinic visits. A wrist heart rate tracker or simple wearable provides:
RPM thus ensures safer, more comfortable aging at home.
After cardiac surgeries or procedures, patients require close monitoring to catch early signs of complications. RPM:
This makes postoperative care safer and more efficient.
Beyond clinical use, RPM technology supports wellness and fitness goals. Devices like an activity tracker that tracks heart rate help users:
These insights encourage healthier habits and informed lifestyle decisions.
A major reason RPM succeeds is its impact on patient involvement. Instead of being passive recipients of care, patients become active participants.
RPM improves engagement through:
This increased involvement boosts adherence to treatments, promotes healthier behavior, and fosters better communication between patients and clinicians.
RPM doesn’t just benefit patients—it also enhances the provider experience by improving workflow, efficiency, and clinical accuracy.
Key advantages include:
After a significant separation, you can incorporate your interlinking keyword:
Many of these digital ecosystems are strengthened by scalable healthcare software development services, enabling providers to streamline operations and support large patient populations effectively.
Though RPM is highly effective, successful implementation requires attention to key challenges:
Healthcare organizations must also ensure compliance with HIPAA and other regional medical data regulations.
The future of cardiac RPM is driven by innovation and expanding digital ecosystems. Upcoming advancements will include:
With further separation, your next interlinking keyword fits naturally:
Advanced ecosystems will integrate with next-generation telemedicine software development, strengthening virtual cardiac management and real-time clinical collaboration.
Remote patient monitoring has completely transformed how heart rate data is captured, analyzed, and used in clinical care. With continuous monitoring tools such as a heart rate tracker, heart rate tracker app, activity tracker with heart rate, heart rate tracker watch, and advanced medical devices, RPM delivers deeper insights than traditional care methods. Combined with intelligent remote patient monitoring software, medical-grade sensors, and AI analytics, RPM improves early detection, enables personalized care, and supports better patient outcomes.
As a leading technology innovator, SISGAIN continues to empower healthcare organizations with advanced remote health monitoring solutions, intelligent RPM platforms, and scalable digital ecosystems that improve cardiac care delivery. With the ongoing evolution of RPM and digital healthcare, heart rate tracking will become even more accurate, accessible, and life-saving shaping the future of cardiology for years to come.
Project quotes, partnerships, implementation
Open roles, referrals, campus hiring