Healthcare Is Becoming Predictive
In 2026, more than 65 percent of large hospital networks globally are using AI-assisted diagnostic tools in radiology, cardiology, or oncology workflows. What was once experimental is now operational. Healthcare is no longer waiting for symptoms to escalate. It is learning to predict them.
For decades, medicine has been reactive. A patient presents symptoms, clinicians investigate, and treatment begins after the condition progresses. Predictive medicine changes that equation. By analyzing longitudinal patient data, behavioral signals, genomics, and real-time monitoring inputs, health systems can identify risk before deterioration occurs. This shift is not incremental. It is structural.
AI-powered predictive healthcare ecosystems combine clinical data, wearable device streams, imaging insights, and population-level intelligence into unified decision frameworks. These systems do not replace physicians. They augment them with probability-based foresight, early warning alerts, and contextual recommendations tailored to each patient.
This transformation sits at the center of the broader AI in Healthcare revolution. From hospital command centers to remote patient monitoring platforms, artificial intelligence is moving care from episodic treatment to continuous intelligence.
In this article, we will move beyond theory. You will gain a practical implementation roadmap, technology stack clarity, real-world use cases, and executive-level insights into how predictive analytics is reshaping personalized care.
From Reactive to Predictive: What Changed?
The shift toward predictive healthcare did not happen overnight. It evolved through three major phases.
First came digitization. Electronic Health Records replaced paper files, creating structured clinical datasets. However, early systems were primarily repositories, not intelligence engines.
Next came analytics. Hospitals began using dashboards, reporting tools, and risk stratification models to analyze historical data. While useful, these systems remained retrospective. They explained what happened but rarely forecasted what would happen next.
Today, healthcare is entering the AI copilot era. Modern systems analyze real-time data streams and provide contextual clinical guidance within physician workflows. This leap has been fueled by an explosion of multimodal data. Genomic sequencing, wearable health monitors, imaging systems, pharmacy records, and social determinants of health now generate continuous inputs. Healthcare data is no longer static; it is dynamic and interconnected.
Cloud infrastructure has enabled scalable processing of this data at enterprise levels. Federated learning frameworks allow institutions to train models collaboratively without sharing sensitive patient data directly, strengthening both performance and privacy.
Regulation has also matured. AI governance boards, model validation protocols, bias audits, and explainable AI requirements are becoming standard in advanced health systems. Transparency and accountability are no longer optional.
These technological and regulatory advances explain why AI is transforming healthcare delivery models globally. Care is shifting from reactive response to predictive orchestration, redefining how outcomes are measured and delivered.
What Is Predictive Analytics in Healthcare? Modern Definition
Predictive analytics in healthcare is no longer limited to statistical forecasting based on historical trends. In 2026, it represents a layered intelligence framework that continuously learns from clinical, behavioral, genomic, and operational data to anticipate risk and recommend timely interventions.
At its core are supervised and unsupervised clinical models. Supervised models are trained on labeled datasets such as confirmed diagnoses, enabling them to predict outcomes like sepsis onset or readmission risk. Unsupervised models, on the other hand, identify hidden patterns within complex datasets, such as unknown patient subgroups or emerging disease correlations.
Risk stratification engines categorize patients based on probability scores, helping clinicians prioritize high-risk individuals. Early warning systems monitor vital signs, lab trends, and contextual patient history to detect deterioration before visible symptoms escalate. Clinical Decision Support 2.0 goes further by embedding these insights directly into physician workflows, offering contextual, explainable recommendations rather than static alerts.
An emerging frontier is digital twin modeling, where virtual replicas of patients simulate treatment responses before real-world intervention, improving precision and safety.
It is important to distinguish between reporting analytics, predictive analytics, and prescriptive analytics. Reporting analytics explains what has happened. Predictive analytics forecasts what is likely to happen. Prescriptive analytics recommends the optimal action to take.
Leading hospital systems worldwide have already deployed AI-enabled sepsis alerts, radiology triage models, and cardiac risk prediction tools, demonstrating measurable reductions in mortality and length of stay. This real-world adoption underscores that predictive analytics is not theoretical innovation. It is operational infrastructure.
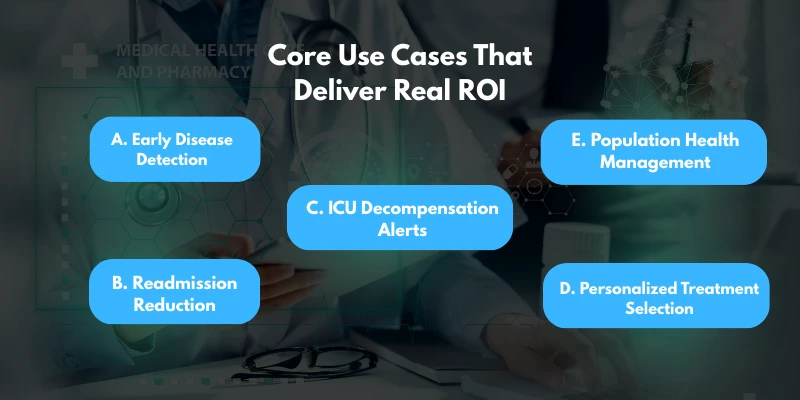
Core Use Cases That Deliver Real ROI
Predictive analytics proves its value when tied directly to measurable outcomes. The following use cases demonstrate how it drives clinical and financial return on investment.
A. Early Disease Detection
In oncology, machine learning models analyze imaging data, pathology reports, and genetic markers to identify malignancies at earlier stages. Early detection improves survival rates and significantly reduces long-term treatment costs.
In cardiology, predictive algorithms assess longitudinal patient data, including cholesterol levels, blood pressure, wearable device metrics, and family history, to forecast cardiovascular events before they occur. Proactive intervention reduces emergency admissions and improves long-term care planning.
B. Readmission Reduction
Hospitals use predictive discharge models to evaluate readmission risk before a patient leaves the facility. By identifying high-risk individuals, care teams can implement targeted follow-ups, medication adjustments, or remote monitoring programs.
This approach aligns with value-based care models, where reimbursement increasingly depends on outcomes rather than service volume. Reducing preventable readmissions directly impacts hospital revenue protection and quality ratings.
C. ICU Decompensation Alerts
In critical care units, context-aware monitoring systems analyze continuous vital sign streams combined with patient-specific baselines. Unlike traditional threshold-based alarms, these systems reduce false positives by incorporating historical and demographic context.
Fewer unnecessary alerts reduce clinician fatigue while enabling earlier intervention for true deterioration events.
D. Personalized Treatment Selection
Genomics combined with AI-driven modeling allows precision drug matching based on individual biological profiles. Instead of trial-and-error prescribing, clinicians can select therapies with higher probability of effectiveness.
This approach reduces adverse reactions, shortens recovery time, and improves therapeutic outcomes.
E. Population Health Management
Payers and large health networks use predictive analytics to identify high-risk population clusters. By analyzing claims data, social determinants, and utilization patterns, organizations can design preventive outreach strategies and personalize coverage policies.
Across all these applications, the objective remains consistent: leverage intelligence to intervene earlier, allocate resources efficiently, and improve measurable outcomes. This is how AI improve patient care at both individual and population levels, translating predictive insight into tangible clinical and financial gains.
The Technology Stack Behind Predictive Healthcare
Predictive healthcare is not powered by algorithms alone. It requires a robust, interoperable, and secure technology architecture that supports clinical-grade intelligence at scale.
At the foundation lies the data layer. Modern systems rely on FHIR and HL7 standards to ensure interoperability across Electronic Health Records, laboratory systems, imaging platforms, and third-party applications. APIs enable structured data exchange between hospital systems, payer platforms, wearable devices, and external registries. Without standardized integration, predictive models remain fragmented and unreliable.
Above this sits cloud infrastructure. Enterprise cloud environments provide scalable compute power for storing and processing massive volumes of multimodal healthcare data. They support distributed training, secure data partitioning, and elastic performance during peak clinical demand.
Model training pipelines form the intelligence core. These pipelines include data preprocessing, feature engineering, validation loops, and continuous retraining mechanisms to prevent model drift. Mature healthcare AI systems also incorporate explainable AI frameworks, ensuring clinicians can understand why a specific risk score or recommendation was generated.
A dedicated cybersecurity layer is essential. Zero-trust architectures, encrypted data pipelines, access governance, and audit trails protect sensitive patient information and maintain regulatory compliance.
Real-time analytics engines process streaming data from ICU monitors, imaging systems, and wearable devices, enabling immediate risk detection. Edge AI capabilities extend intelligence to remote patient monitoring environments, allowing devices to analyze data locally before securely syncing with centralized systems.
Building and orchestrating this ecosystem requires deep domain expertise. Hospitals must collaborate with experienced AI Development Companies that understand regulatory standards, clinical validation requirements, and large-scale system integration. Predictive healthcare is not a software feature. It is enterprise infrastructure.
Implementation Roadmap for Hospitals
Adopting predictive analytics requires structured execution rather than isolated experimentation. A phased roadmap ensures clinical reliability, regulatory compliance, and measurable return on investment.
Phase 1: Data Audit and Governance
Hospitals begin by conducting a comprehensive data maturity assessment. This includes evaluating data completeness, quality, interoperability, and standardization levels. A compliance review ensures alignment with privacy regulations and institutional policies. Identifying interoperability gaps across EHR systems, diagnostic platforms, and external providers prevents integration delays later in the process.
Phase 2: Use Case Prioritization
Not every predictive model delivers equal impact. Leadership teams must identify high-value use cases aligned with institutional strategy. ROI modeling helps quantify cost avoidance, readmission reduction potential, and operational efficiency gains. Clinical validation planning ensures chosen use cases have measurable endpoints and physician sponsorship.
Phase 3: Model Development and Validation
During this stage, data scientists and clinical experts collaborate to develop and train predictive models. Clinical testing in controlled environments validates accuracy and safety. Bias detection protocols evaluate performance across demographic groups to prevent inequitable outcomes. Algorithm transparency mechanisms are implemented to ensure explainability and clinician trust.
Phase 4: Integration with Healthcare Software
Successful models must be embedded into daily workflows. Integration with EHR systems ensures recommendations appear at the point of care. Workflow optimization reduces alert fatigue and enhances usability. Structured staff training programs prepare clinicians and administrators to interpret predictive outputs confidently.
Throughout this process, alignment with broader healthcare softwre solutions strategies ensures that predictive systems operate seamlessly within existing digital ecosystems. Hospitals that follow this structured approach move beyond pilot projects and establish predictive intelligence as a sustainable operational capability.
Key Challenges in 2026
Predictive healthcare in 2026 faces far more sophisticated challenges than those discussed a decade ago. The conversation has shifted from data availability to accountability, reliability, and ethical deployment.
AI bias and fairness remain central concerns. Models trained on non-representative datasets may underperform in diverse populations, leading to inequitable risk predictions. Health systems must conduct demographic performance audits and continuous bias monitoring to ensure equitable outcomes across age groups, ethnicities, and socioeconomic backgrounds.
Model drift is another operational reality. Clinical practices evolve, patient demographics shift, and disease patterns change. Without continuous retraining and validation, predictive models degrade over time. Mature institutions now implement monitoring dashboards that track performance metrics in real time and trigger recalibration when thresholds are breached.
Regulatory oversight has also intensified. AI governance boards, mandatory validation documentation, and explainability standards are becoming institutional norms. Health authorities increasingly require transparency into how risk scores are generated, especially when models influence treatment decisions.
Data privacy expectations have risen alongside cyber threats. Zero-trust architectures, granular access controls, and encrypted data flows are no longer optional. Predictive ecosystems must protect patient data across cloud, on-premise, and edge environments.
Clinician resistance remains a human challenge. Physicians may question algorithm reliability or fear loss of autonomy. Transparent design, contextual alerts, and collaborative validation processes are critical for adoption.
Finally, liability in AI-assisted diagnosis presents legal complexity. Clear governance policies must define accountability boundaries between clinicians, institutions, and technology providers. Addressing these realities demonstrates that predictive healthcare is not merely technological innovation but responsible system transformation.
The Role of AI Development Expertise
While predictive healthcare offers transformative potential, hospitals cannot build and scale these systems casually or entirely in-house. Healthcare environments demand clinical precision, regulatory compliance, and long-term operational sustainability.
Developing predictive models requires interdisciplinary collaboration between clinicians, data scientists, security architects, and regulatory experts. Many hospitals lack the internal infrastructure, scalable engineering capacity, or AI lifecycle management frameworks to execute this independently.
Blind experimentation in live clinical settings is not an option. Patient safety demands controlled validation environments, bias audits, model explainability, and rigorous documentation before deployment.
This is where specialized AI Development Services become critical. Experienced partners bring domain-specific healthcare knowledge, familiarity with compliance frameworks, and proven validation methodologies. They understand how to design models that integrate seamlessly with EHR systems and operational workflows.
Equally important is scalable architecture planning. Predictive systems must handle growing data volumes, regulatory updates, and continuous model retraining without disrupting clinical operations. Collaboration with a mature App development Company ensures that predictive intelligence is embedded into secure, user-friendly applications rather than existing as isolated analytical tools.
In predictive healthcare, expertise is not optional. It is foundational to safe, compliant, and scalable transformation.
ROI and Financial Impact of Predictive Healthcare
Predictive healthcare is not simply a clinical upgrade. It is a financial strategy aligned with modern reimbursement and operational models.
One of the most immediate gains comes from reduced readmissions. By identifying high-risk patients before discharge and implementing targeted follow-up interventions, hospitals lower penalty exposure and protect reimbursement under value-based care programs. This represents direct cost avoidance and measurable margin protection.
Predictive models also reduce unnecessary diagnostics. Context-aware risk scoring helps clinicians avoid redundant imaging, excessive lab testing, and defensive medicine practices. Over time, this improves resource allocation while maintaining clinical quality.
Improved bed utilization is another strategic advantage. Early discharge risk prediction and ICU deterioration forecasting optimize patient flow, reduce bottlenecks, and increase throughput without infrastructure expansion. For large hospitals, even small improvements in occupancy management translate into significant operational efficiency gains.
Preventative care strategies powered by predictive analytics reduce long-term treatment expenses. Early identification of chronic disease risk lowers the burden of emergency interventions and complex inpatient care.
As reimbursement shifts toward outcome-driven revenue models, predictive systems become revenue enablers rather than cost centers. Institutions that demonstrate measurable improvement in quality metrics, readmission rates, and patient outcomes are better positioned to negotiate payer contracts and strengthen financial sustainability.
The Future: 2026 to 2030 Outlook
Between 2026 and 2030, predictive intelligence will move from optional innovation to foundational healthcare infrastructure.
AI copilots embedded directly into EMRs will provide contextual decision support at the point of care. Rather than navigating separate dashboards, clinicians will receive real-time risk assessments, treatment suggestions, and evidence-backed recommendations within their existing workflow environments.
Personalized medical policies are likely to emerge as payers leverage predictive analytics to tailor coverage decisions based on individual risk profiles and treatment effectiveness patterns. This shift will redefine how benefits are structured and reimbursed.
AI-powered digital twins will simulate patient-specific treatment pathways, enabling clinicians to evaluate probable outcomes before initiating therapy. This capability will expand precision medicine beyond oncology into cardiology, endocrinology, and complex chronic disease management.
At a macro level, predictive national health systems will deploy real-time population risk dashboards to anticipate outbreaks, manage chronic disease burdens, and optimize public health resource allocation.
The integration of AI and IoT remote patient ecosystems will enable continuous monitoring beyond hospital walls, transforming episodic care into longitudinal health management.
The trajectory is clear. Healthcare is evolving toward a continuously learning, predictive ecosystem where intelligence operates at individual, institutional, and national levels.
Strategic Closing: From Data to Decisions
Healthcare is moving toward a future where predictive intelligence is no longer a competitive advantage but a baseline expectation. Within the next few years, data-driven foresight will become embedded into standard clinical operations. Hospitals that embrace this shift will operate with greater precision, efficiency, and resilience. Those that delay risk falling behind in both clinical outcomes and financial performance.
AI-driven personalization should not be viewed as experimental innovation. It is emerging as core infrastructure, much like EHR systems once were. Predictive models, contextual decision support, and real-time risk stratification will define how care is delivered, reimbursed, and evaluated.
The question for healthcare leaders is no longer whether predictive analytics will shape the industry. The question is how strategically and responsibly it will be implemented within their institutions.
Forward-thinking organizations are already aligning governance, technology, and clinical leadership around this transformation. A structured, expert-led approach ensures that predictive systems are not only powerful but safe, compliant, and sustainable.